The Five Second Glasses Test That Predicts a Dry Eye Day
I have spent an embarrassing amount of time thinking about dryness.
Not just dry eye as a condition, but environmental dryness. The kind that quietly sabotages your eyes over the course of a day while you are locked in a staring contest with your computer screen, also known as answering emails.
Like most eye care providers, I have read, written, and recommended the standard dry eye advice. Blink more. Use artificial tears. Adjust your workstation. Stay hydrated. All of it is valid. None of it directly answers the question that has one of the greatest influence on ocular hydration over the course of a day.
How dry is today, really?
Not in theory. Not according to a weather app. But in the exact space where you are sitting right now.
Why predicting dryness is harder than it sounds
At one point, I tried to solve this properly.
I wrote code that pulled local temperature and humidity data. I cross referenced it with in clinic measurements of tear film instability. The idea was to predict ocular dryness stress for a given day, the way we predict UV index or pollen counts.
It worked beautifully until it didn’t. One unusually rainy month in Calgary, with humidity levels off the charts, completely broke the model. On paper, conditions looked ideal. In reality, patients were complaining about dryness more than ever. The reason turned out to be simple. Everyone was indoors, sealed into buildings with air blowing directly across their faces.
The model wasn’t accounting for how people actually live and work. Most of us are not spending our days outside, faithfully experiencing the weather data predicted by our phones. And we are also not sitting in buildings that are just slightly warmer or colder versions of the outdoors.
Buildings have HVAC systems. Some add humidity. Some strip it out. Many do both depending on the season. Almost all of them introduce airflow, which turns out to matter just as much as humidity itself.
Every workspace is different. Sitting under a heat vent is not the same as sitting next to a window. An office tower downtown is not the same as a home office near a fireplace. Two people in the same building can experience completely different drying forces depending on where they sit. Once you factor in all of that, the idea of predicting dryness from outside weather alone collapses pretty quickly.
There are too many variables, and too many of them are personal.
Dryness is cumulative, not dramatic
Dry eye usually does not show up suddenly. It builds. Your tear film is only a few micrometers thick, and it starts evaporating immediately after every blink. If evaporation is slightly faster than normal for hours at a time, the surface becomes stressed long before you feel obvious symptoms.
By the time your eyes burn at night, the damage is already done. Adding artificial tears then helps, but it is late in the process. The real advantage is catching drying conditions early in the day and responding before tear film instability stacks up.
The problem is that humans are terrible at sensing evaporation directly. Your eyes compensate. Vision often degrades before discomfort appears.
Then I tripped over something extremely low-tech.
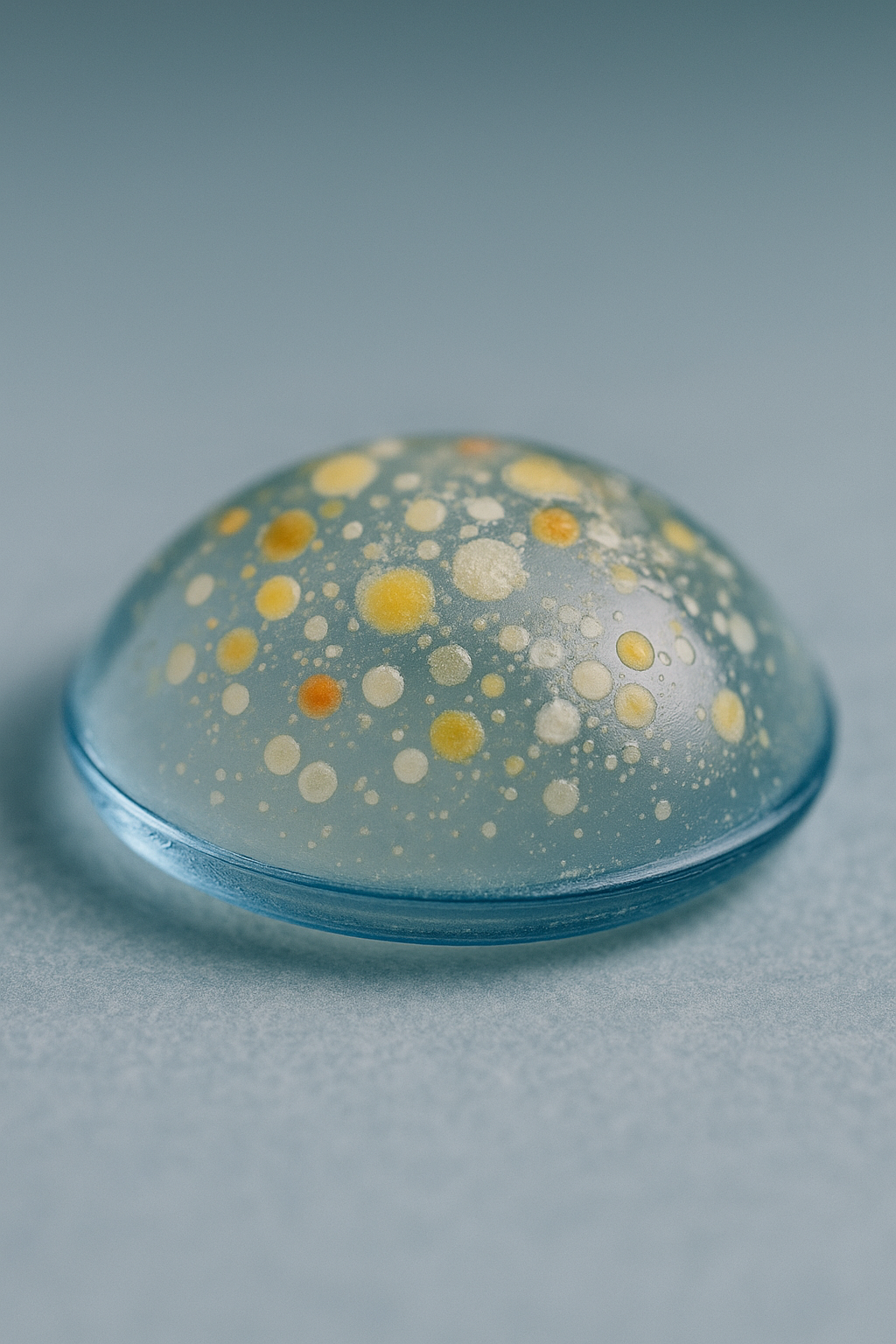
When you breathe on your glasses, warm humid air hits a cooler surface. Water condenses. The lens fogs. You have done this thousands of times without thinking about it. What happens next is the important part.
The surrounding air pulls that moisture away. How fast the fog disappears depends on how aggressively the environment wants water. Humidity matters. Airflow matters. Temperature matters. All the same forces that act on your tear film are suddenly playing out in front of you, in a way you can actually see.
The glasses fog test
This is not a medical test. It is much simpler, and possibly more useful.
Breathe evenly on your glasses until they fully fog.
Start counting.
Stop when the fog is completely gone.
That is the entire test.
The number itself does not matter. What matters is comparison. Same glasses. Same person. Different environments. Your office versus your home. Morning versus afternoon. Winter versus summer. One building versus another. If the fog disappears noticeably faster than it usually does, the current environment is more drying than the ones where your eyes are usually exposed to. And if disappears slower, its less drying.
Yes, lens coatings affect fog behavior. Anti reflective layers and scratch resistance change how water spreads and evaporates.
That turns out not to matter much if you are using your own glasses as your reference. You are not trying to measure absolute dryness. You are answering a more practical question.
Is this environment pulling moisture away faster than the environments my eyes are usually exposed to?
That single comparison cuts through all the complexity that made modeling dryness impossible in the first place. It automatically accounts for airflow. It accounts for local humidity. It even accounts for the fact that your desk might live under a vent that operates with all the subtlety of a Dyson hair dryer pointed directly at your eyeballs.
Why this is useful for dry eye management
Dryness is cumulative. If tear evaporation is accelerated all day, tear film breakup happens sooner after every blink. That happens hundreds of times an hour. By evening, the surface is already irritated and unstable.
If you wait until bedtime to react, you are treating the aftermath. The glasses test can give you an early warning: This is a high evaporation environment. Today is a drying day. This is not a wait and see situation.
That is the moment when increasing artificial tear frequency actually makes a difference. Not because your eyes feel bad yet, but because you are preventing the cascade that leads to symptoms later. On days when the fog lingers longer than expected, your baseline routine may be enough.
It turns dry eye care from reactive to predictive, which is where it works best.
What this test does and does not do:
It does not diagnose dry eye.
It does not measure tear quality.
It does not replace an eye exam.
It does not allow comparison between people.
What it does do is give you a surprisingly clear sense of how hard your environment is working to pull moisture away from your eyes.
Dr. Robert Burke is an optometrist at Calgary Vision Centre. The thoughts, opinions, and analogies shared above are intended for education and entertainment purposes only (think of them like a friendly explainer, not a personal consultation.) Every set of eyes is different, and the right testing protocol depends on your specific vision needs, health history, and lifestyle. So if you're experiencing symptoms or just have questions about your vision, don’t rely on internet content alone, talk to your optometrist or health care provider directly. We’re here to help, but nothing beats an in-person exam with someone who knows your eyes.