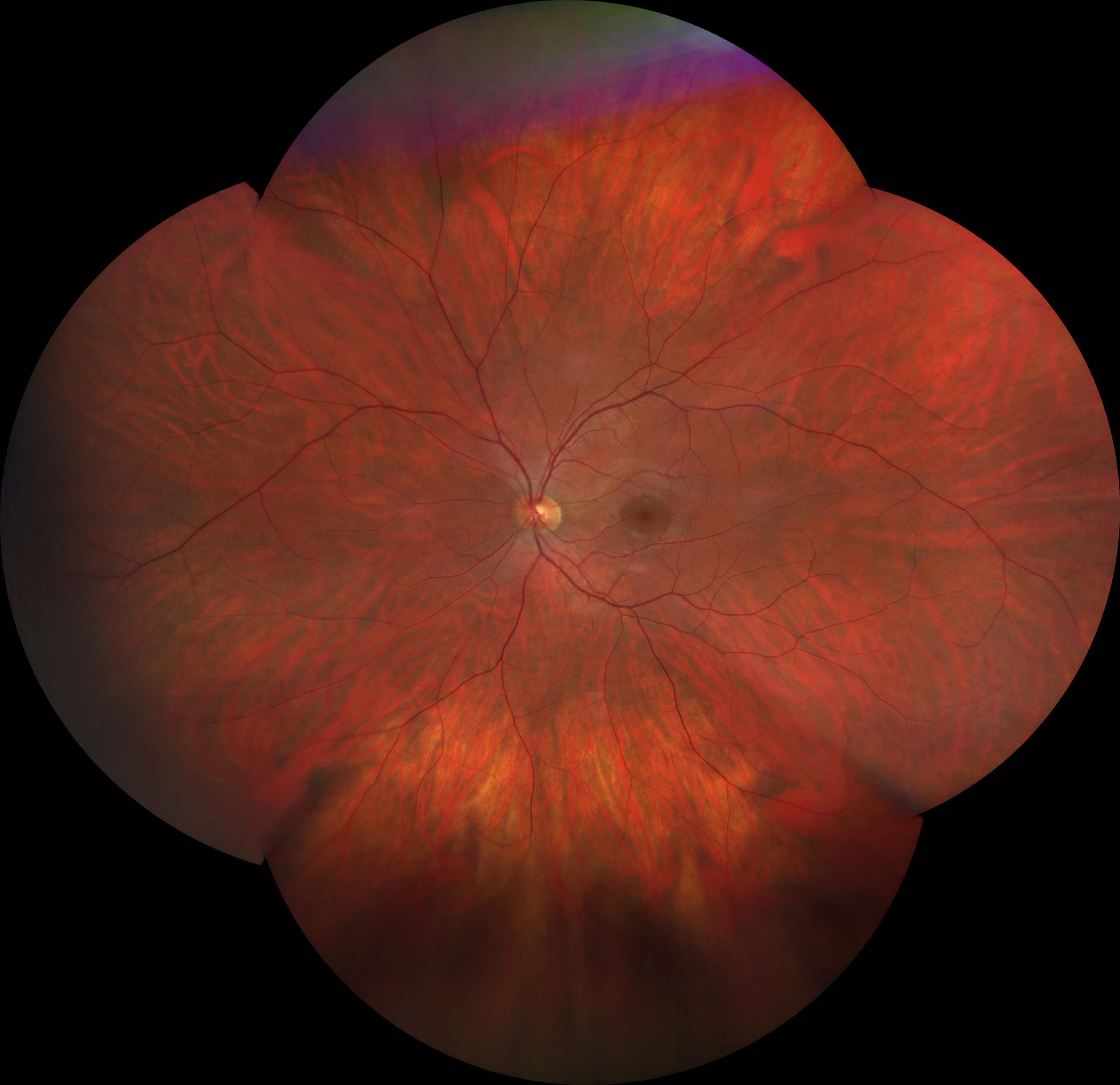
Figure 1: A patients retinal image captured at Calgary Vision Centre March 22, 2018.
The image above is an actual image captured in our clinic by our equipment and rendered in office.
The orange "stuff" in the image above is the retina which is the photoactive tissue lining the inside of our eyeballs. It is extremely important to eyesight, and is very fragile. Because humans only have one small hole allowing light into the eye (the pupil) it is very difficult to visualize the retina in most circumstances. The most basic retinal screening would be when you utilize flash photography and the subject of your photo has "red eye". The red is actually a reflection of the retina bouncing out of the pupil, and although you can't tell much from this, at least you can say that your subject has a retina. To see the retina in any real detail can be challenging as the pupil is naturally small and gets even smaller when light is shone into it. This is why when there is any concern with the retina, an eye must be dilated (put drops in to make the pupil larger), allowing a better view of the tissue inside. A dilated retinal exam is still the gold standard for viewing the retina, but the problem is that it's time consuming, can cause certain types of glaucoma in at-risk people, and patients don't particularly enjoy being light sensitive and unable to focus up close for 4-6 hours while the drops are wearing off. This is why dilation is not routinely done on screening eye exams. Therefore it's important to have different ways to views the retina when the eye is undilated to help screen for cases where dilation is warranted.
The patient's eyeball in Figure 1 (above) has been routinely imaged in our clinic since 2004, and as you will see below, the way we examined and recorded the results (when undilated) has change drastically in the last 15 years, a time frame which we can divide it four major eras of imaging technology. At the start of each era, our clinic was consistently one of the country's very earliest adopters of each new tech.
analog era
pre - 2005
digital era
2005 - 2011
3D era
2011 - present
ultrawide era
2018 - present
THe Analog era (Pre - 2005)
A handheld light called an ophthalmoscope is shone into the eye. The device creates a small spotlight on the retina, and the doctor needs to move the spot around to view a larger swath of tissue. Due to the device lacking any imaging capabilities, any pertinent findings are usually recorded via a crude sketch. When your family doctor looks into your eye, this is what they are doing. Due to being cost effective and portable, the hand held opthalmoscope is still very popular in clinics worldwide. The drawing on the right represents the results of undilated opthalmoscopy on our patient from Figure 1, and as you can see, the results of which show little resemblance to each other (though not technically inaccurate).
Area of retina seen: 20° (after numerous sweeps of the light)
The Digital era (2005 - 2011)
The acquisition of a colour retinal camera was a significant step forward for us, not only in diagnostic capabilities but also in accuracy of record keeping. Having one colour image of some very important parts of the retina to be able to exam as close as needed, and to refer back to at a later date, was at the time truly amazing.
The retinal tissue captured in this image is starting to resemble the retina in Figure 1, and a trained clinician would be able to see similar blood vessels and structures between the two. However the field of view captured in this image is still fairly small as edge-to-edge in this image only represents about a 30° area of the retina. All the black surrounding the image is more retina that is unable to be seen by this technology. For reference, the yellow circle in the centre of this image is the optic nerve, and when you cross-reference the optic nerve to Figure 1, you can see how zoomed in this photo is.
Area of retina seen: 30° in a colour image.
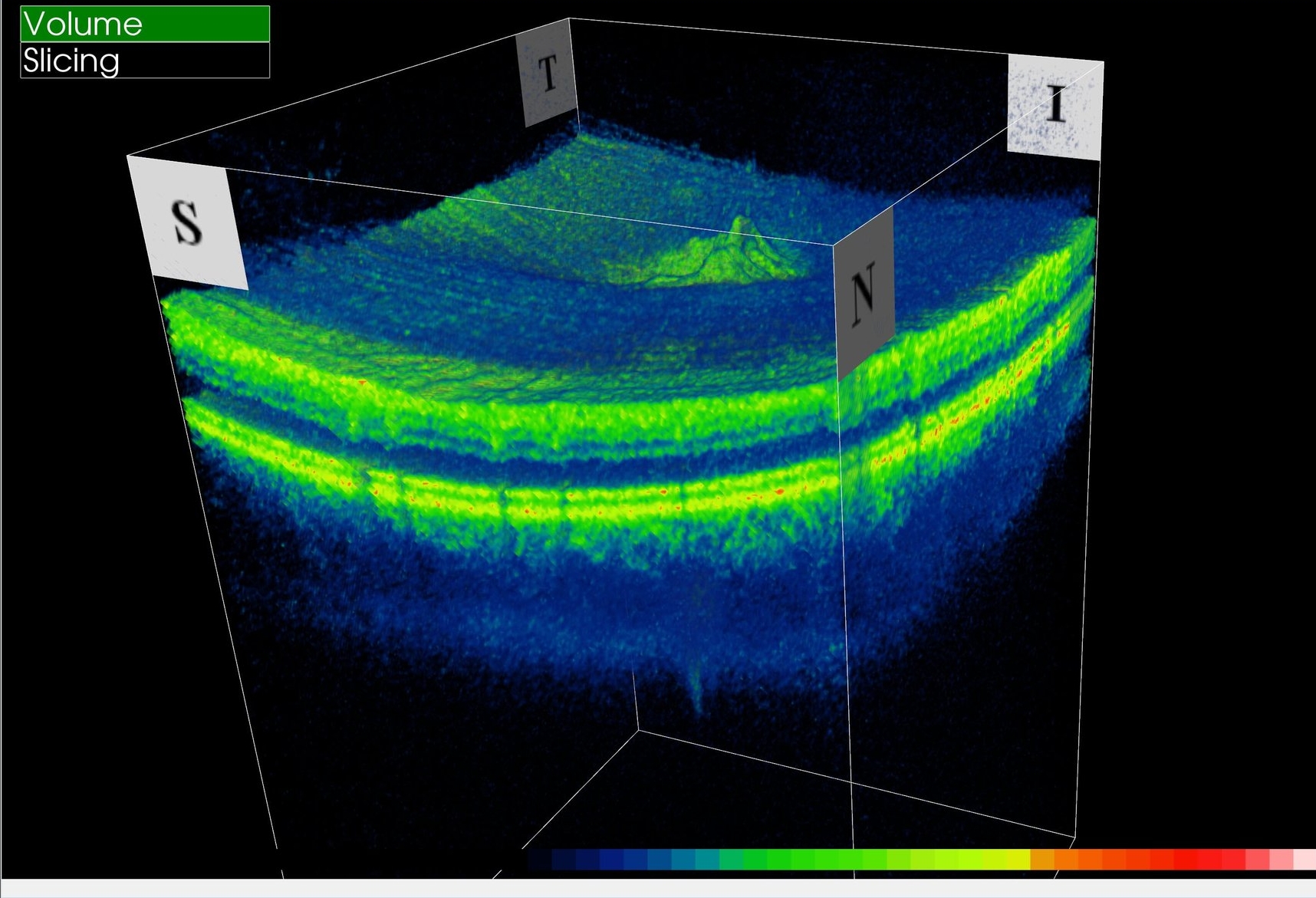
The 3D Era (2011 - present)
Currently, we are still in the Topcon 3D OCT-2000 era and while this technology doesn't expand our field of view any further past the 30° mark, it does have the amazing ability to gather sub-surface, depth, and elevation data in this zone. In addition, it is able to measure and track the size of certain structures automatically, while cross referencing these value to a normative database to flag any concerns.
Area of retina seen: 30° in a colour image that includes sub-surface, depth, and elevation data.
The ultra-wide field era (2018 - present)
With the 3D era being so revolutionary in terms of diagnosing and tracking any changes in a specific area of the retina, the ultra-wide field era has been created to supplement this data by allowing us to venture, for the first time, to parts of the retina located outside of the historical 30° zone. In the image above, the same area of the retina is represented before and after the installation of the Zeiss Clarus 500 ultra-wide field camera. It's quite amazing how much more of the retina this camera can capture than it's predecessors, all while maintaining true colour, which is important in being able to diagnose concerning freckle-like lesions. In addition this camera also has the ability to show areas of imminent cell death by using a feature called 'fundus auto-fluorescence' which is remarkable.
The image used in Figure 1 is this ultra-wide montage photo collected by the Zeiss Clarus 500, combined with data from the Topcon 3D OCT, and rendered in-office.